COVID-19 Vaccine and Cancer Risk: Summary of Current Evidence
Two large national studies recently reported that people who received COVID-19 vaccines were diagnosed with cancer more often than those who did not. The increase was seen across multiple vaccine types and cancer types, and the pattern remained consistent even after accounting for age, income, and health conditions.
These findings do not prove that vaccines cause cancer, but they show a clear pattern that deserves further investigation. This article reviews the data so readers can understand what was measured, what was found, and what actions may be worth considering.

New Studies Link COVID-19 Vaccines to Higher Cancer Risk
New evidence is drawing attention to the possible link between COVID-19 vaccination and cancer risk.Two recently published large-scale population studies, one in Italy and another in South Korea, have raised important questions about the long-term safety of COVID-19 vaccines, particularly mRNA-based platforms. Both studies reported consistent signals of elevated cancer risk among vaccinated populations compared to unvaccinated groups.
What makes these findings especially significant is that they represent the first population-wide cohort studies to examine vaccine safety in relation to cancer risk. Coming from two independent nations with different health systems, the Italian and South Korean studies corroborate each other’s results, providing one of the strongest signals to date that long-term cancer incidence may be affected by COVID-19 vaccination.
Cancer Risks Identified by Vaccine Platform
To put the new data into perspective, researchers reported measurable increases in cancer risk by vaccine type after one year of follow-up:
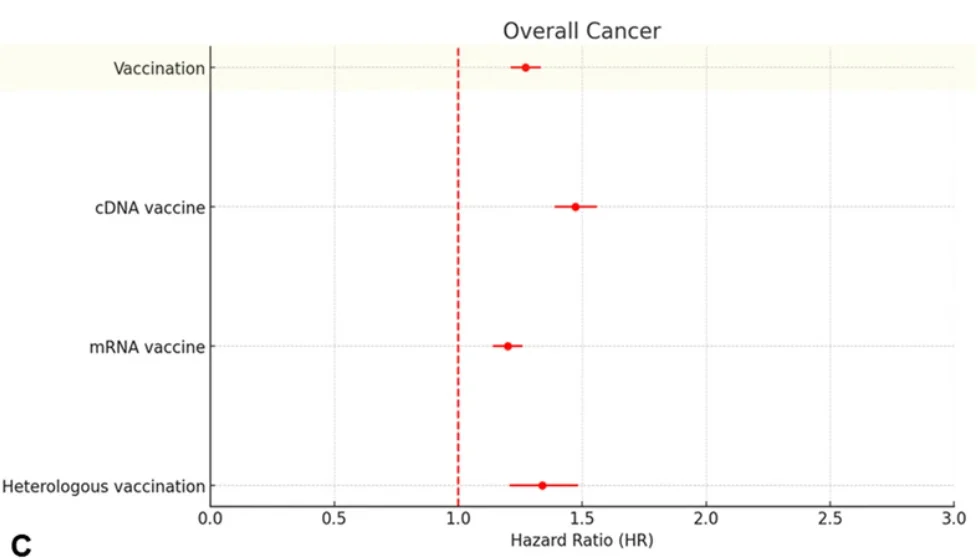
- Viral-vector (cDNA) vaccines: +47%
- Mixed schedules: +34%
- mRNA vaccines: +20%
In these studies, cancer risk was measured using hazard ratios (HRs), a standard method for comparing the rate of an outcome between two groups. An HR above 1.0 indicates an increased risk in the vaccinated group compared to the unvaccinated. For example, an HR of 1.20 reflects a 20% higher incidence of cancer in the vaccinated population. This method ensures that results are statistically meaningful rather than coincidental.
Key Takeway: No matter which type of COVID-19 vaccine people received, vaccinated individuals were diagnosed with cancer more often than unvaccinated individuals within a year. The size of the increase depended on the vaccine type, but none of them showed zero risk.
Study Design at a Glance (South Korea)
- Population: 8,407,849 adults
- Database: Korean National Health Insurance (2021–2023)
- Methodology: Retrospective cohort with propensity score matching (1:4 vaccinated vs. unvaccinated)
- Adjustments: Age, sex, comorbidities, income level, prior infection
- Outcome Window: 1-year incidence of overall and site-specific cancers
Key Takeway: This study followed more than 8 million adults and made sure vaccinated people were compared only to unvaccinated people with similar health, age, and income. This means the higher cancer rates cannot easily be explained away by lifestyle differences.
Cancer Outcomes Reported in the South Korean Study
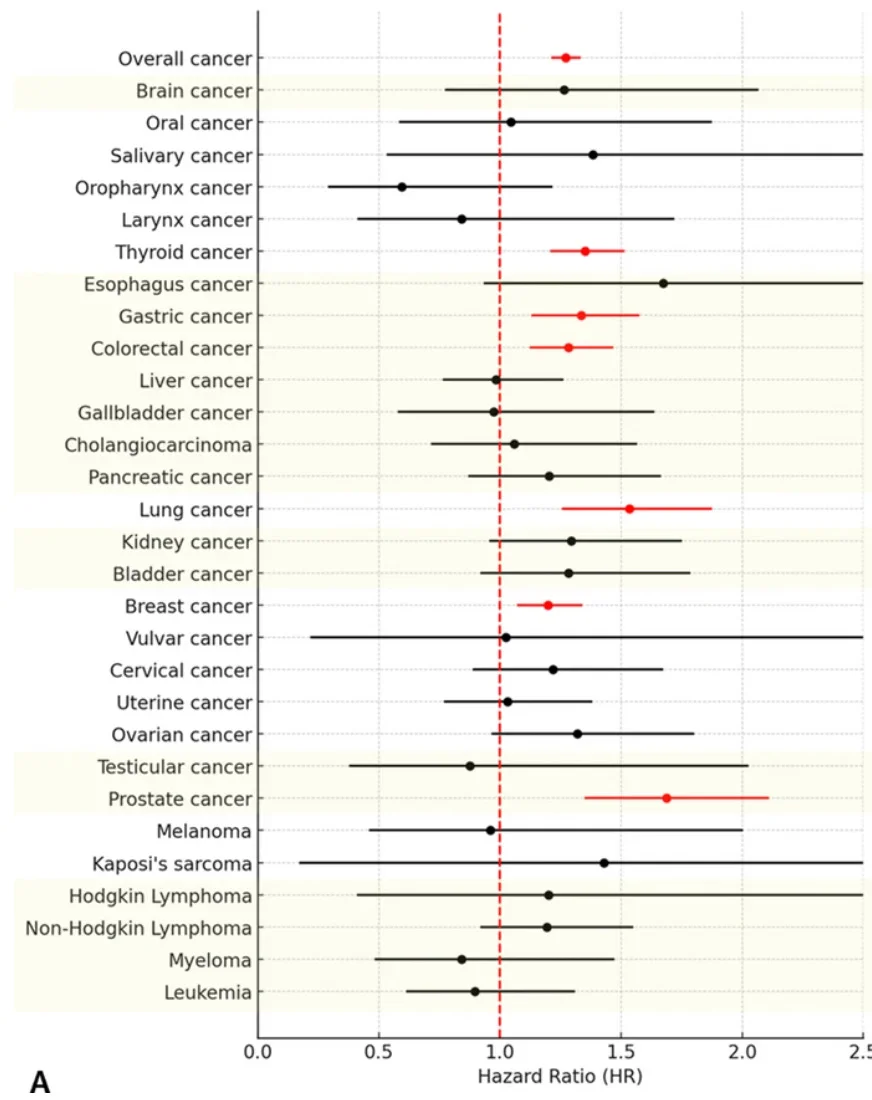
The South Korean cohort study of 8.4 million adults provided additional detail on specific cancer outcomes within one year of vaccination:
- Overall cancer risk: 27% higher in vaccinated vs. unvaccinated
- Lung cancer: 53% higher risk
- Prostate cancer: 69% higher risk
- Thyroid cancer: 35% higher risk
- Gastric cancer: 34% higher risk
- Colorectal cancer: 28% higher risk
- Breast cancer: 20% higher risk
To put these numbers in context, an HR of 1.53 for lung cancer means vaccinated individuals developed lung cancer at a rate 53% higher than matched unvaccinated peers over the same one-year follow-up period. Similar interpretations apply to each cancer type above.
Key Takeway: Vaccinated people were diagnosed with several major cancers—such as lung, prostate, thyroid, stomach, colon, and breast cancer—more often than unvaccinated people within one year of follow-up.
Cancer Risks Across Demographics
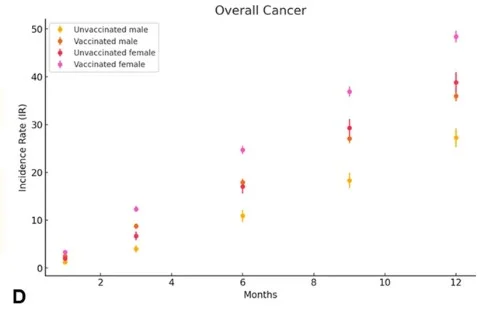
The elevated cancer risks were not confined to one group, they appeared across all demographics, though the type and severity varied:
- Women: higher risks for thyroid and colorectal cancers
- Men: higher risks for gastric and lung cancers
- Elderly adults (≥75 years): greatest absolute burden, especially prostate cancer
- Younger adults (<65 years): increased risks for thyroid and breast cancers
The researchers also reported absolute case numbers, showing the burden in real-world terms. For women, cancer incidence was 48.4 per 10,000 vaccinated versus 38.2 per 10,000 unvaccinated. Among elderly adults (≥75 years), the rates climbed to 119.9 per 10,000 vaccinated compared to 91.7 per 10,000 unvaccinated. These figures highlight that women and older adults carried the heaviest burden, though younger adults also experienced clear increases in thyroid and breast cancers.
Key Takeaway: The increase in cancer was seen in men, women, younger adults, and seniors. The specific cancer types differed depending on the group, but no age or gender appeared fully unaffected.
Booster Dose Impact
Booster doses raised additional concern, with the data showing a more than two-fold increase in pancreatic cancer risk (South Korean cohort study).
- Pancreatic cancer: HR 2.25 → a more than two-fold increase in risk (125% higher).
- Gastric cancer: HR 1.23 → a 23% higher risk compared to non-boosted individuals.
These booster findings came from analyses that compared boosted individuals to non-boosted individuals within the vaccinated group. The more than two-fold increase in pancreatic cancer risk (HR 2.25) was particularly striking, given that such a sharp rise suggests a strong signal rather than random variation.
What this shows is clear: no vaccine platform was free of risk. Every technology studied—mRNA, viral-vector, or mixed—was linked to a statistically significant increase in overall cancer incidence within just one year.
Key Takeway: People who received booster doses showed even higher cancer rates than those who only received the original shots. In some cases, such as pancreatic cancer, the increase was more than double.
Italian Study: Longer-Term Findings
The Italian population study followed nearly 300,000 residents over a 30-month period, making it the longest-running dataset to date on COVID-19 vaccines and cancer risk. Researchers found that long-term cancer incidence was elevated after mRNA vaccination, with significant increases in overall cancer, breast cancer, bladder cancer, and colorectal cancer.
Unlike the South Korean study, which focused on a one-year follow-up, the Italian cohort tracked residents for 30 months, offering a longer-term perspective. This extended dataset suggests that increased cancer risks may persist or even evolve over time, reinforcing the importance of monitoring long-term outcomes.
Key Takeaway: Over a longer period of 30 months, vaccinated people continued to show higher cancer rates, especially breast, bladder, and colon cancer, suggesting the increase may not fade over time.
Protecting Your Health After COVID-19 Vaccination
Although more research is needed to confirm causation, current evidence suggests that mRNA and other COVID-19 vaccine platforms have been consistently associated with higher cancer incidence in large population studies. This raises important considerations for both patients and practitioners. At Internal Healing & Wellness MD, we believe science must remain transparent, open, and willing to revisit assumptions when new data emerges.
Understanding potential risks allows patients to make informed decisions and to pursue proactive, functional medicine strategies that support immune system resilience, cellular detoxification, and cancer recovery and prevention.
At Internal Healing & Wellness MD, we also recognize the need for a functional medicine perspective on these findings. By focusing on root causes, supporting detoxification, and strengthening immune defenses, patients can take proactive steps to lower their risk. This includes evaluating how COVID-19 vaccines may affect immune resilience and tailoring personalized care to restore balance.
Exploring Functional Medicine and Repurposed Therapies for Cancer Prevention
Alongside emerging vaccine safety data, researchers are investigating whether certain repurposed therapies may offer broader health benefits, particularly in oncology.
Early evidence suggests that compounds such as:
- Ivermectin, traditionally used as an antiparasitic, is now being evaluated for its potential role in cancer treatment.
- Mebendazole, another antiparasitic, has shown promising anti-tumor activity in early studies.
These therapies are considered safe, affordable, and worthy of continued investigation as part of a comprehensive functional medicine approach to cancer prevention and recovery, and long-term wellness.
We help patients integrate strategies like functional medicine testing, detoxification support, and metabolic optimization protocols to support both prevention and recovery.
Staying Proactive About COVID-19 Vaccine and Cancer Risk
With two independent national datasets converging on the same conclusion, the evidence cannot be ignored. While these studies do not prove causation, they show a consistent association between COVID-19 vaccination and elevated cancer incidence across multiple platforms and demographics. Given that nearly 70% of the global population has received these vaccines, the implications for long-term public health are profound and demand ongoing investigation.
Public health data is complex, and ongoing research will continue to refine our understanding of COVID-19 vaccine safety and cancer risk.
What remains clear is the importance of a personalized approach to health care—one that considers genetic predisposition, immune resilience, lifestyle, and evolving scientific data.
What Observational Studies Can (and Can’t) Prove
The studies discussed in this article are observational, meaning researchers looked back at existing medical records and compared vaccinated people to unvaccinated people. This type of research is valuable because it can detect patterns across millions of people in real-world conditions. However, it also has limitations.
Because people were not randomly assigned to receive or skip vaccination, there may be differences between groups that cannot be fully controlled for, even when adjustments are made for age, income, or health status. This is why observational studies can show a strong association but cannot formally prove cause and effect.
The only way to confirm causality with high certainty would be through long-term randomized controlled trials, where participants are assigned by chance to receive or not receive an intervention. Such trials are slower, more expensive, and often smaller in size, which is why data like this usually appears first in observational studies.
In other words, the current findings are strong signals that warrant further investigation, not final conclusions.
Frequently Asked Questions
Current studies do not prove causation but have found consistent associations between vaccination and higher cancer incidence in large populations. Researchers emphasize these findings as signals that require further investigation, not final conclusions.
The South Korean study reported a hazard ratio (HR) of 1.27 for overall cancer. This means that vaccinated individuals developed cancer at a rate 27% higher than unvaccinated peers during the same one-year period, after adjusting for age, sex, and other factors. A hazard ratio does not prove causation but reflects a measurable difference in incidence.
Both vaccine platforms showed measurable increases in cancer incidence. The Italian study found that mRNA vaccines were associated with overall cancer, breast cancer, bladder cancer, and colorectal cancer. The South Korean study showed that viral-vector (cDNA) vaccines were linked to higher risks of thyroid, gastric, lung, and prostate cancers. No vaccine platform appeared risk-free in the available data.
The South Korean study found booster doses were associated with additional cancer risks. Pancreatic cancer risk more than doubled (HR 2.25), and gastric cancer risk increased by 23% compared to those who did not receive boosters. These findings suggest that additional doses may compound certain site-specific risks, though further research is needed.
The South Korean study showed that elevated risks appeared across all groups, but with some differences. Women had higher risks for thyroid and colorectal cancers, while men had increased risks for gastric and lung cancers. Older adults (≥75 years) carried the greatest absolute burden, especially for prostate cancer, while younger adults under 65 also experienced elevated risks, particularly thyroid and breast cancers.
Functional medicine focuses on strengthening the body’s defenses through advanced diagnostic testing, detoxification support, immune resilience strategies, and integrative therapies. These approaches may help patients support both prevention and recovery.
If you are concerned, speak with a healthcare provider who can assess your individual risk profile. At Internal Healing & Wellness MD, we use functional medicine testing, detoxification support, and personalized care plans to help patients strengthen resilience and support long-term health.
Take the Next Step Toward Protecting Your Health
If you are concerned about how vaccine data may affect your health, we encourage you to book a consultation. Together, we’ll review your individual risk profile and create a personalized strategy to strengthen your long-term health and wellness.
References
Kim, J., et al. (2025). 1-year risks of cancers associated with COVID-19 vaccination: a large population-based cohort study in South Korea. Biomarker Research.
https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00831-w
Silvestris, N., et al. (2025). COVID-19 vaccination, all-cause mortality, and hospitalization for cancer: 30-month cohort study in an Italian province. PubMed.
https://pubmed.ncbi.nlm.nih.gov/40881928/
COVID-19 vaccinations worldwide. Our World in Data.